Find Relief From Bowel Control Problems!
As board certified colorectal surgeons, we have comprehensive solutions proven to help reduce the symptoms of fecal incontinence. From conservative options, to medications, and advanced therapies, our practice is focused on tailoring a treatment plan for your unique needs.

About Us
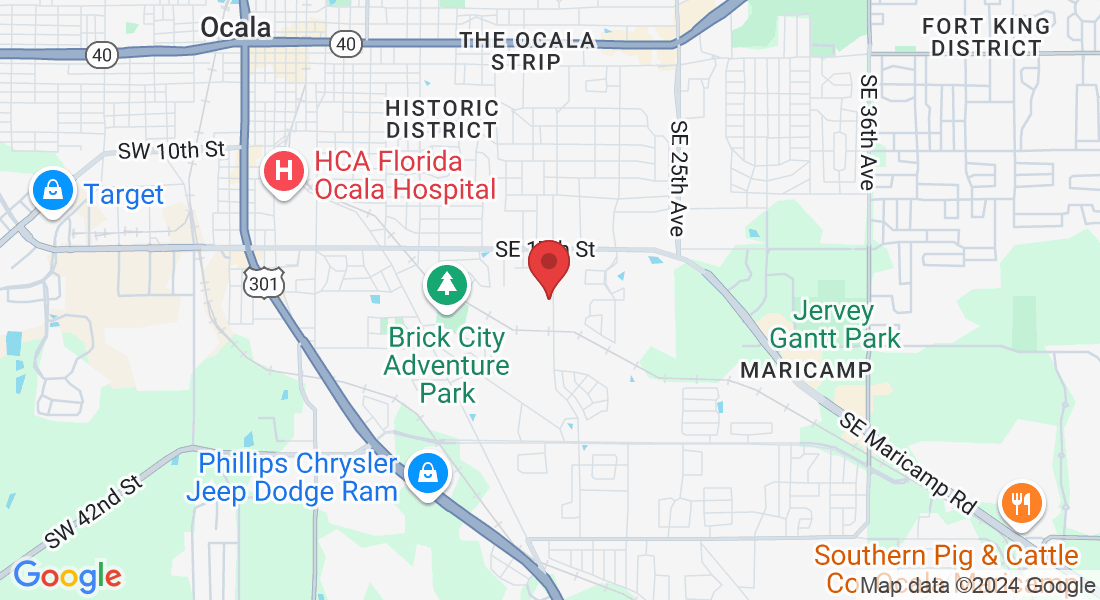
Welcome to Surgical Consultants of Central Florida, where excellence in bowel control care meets compassionate patient-centered service. Our practice comprises a team of highly specialized colorectal surgeons dedicated to treating bowel control problems with precision and expertise. What sets us apart is our commitment to delivering personalized care tailored to each patient's unique needs. Whether it's through advanced diagnostic techniques or innovative treatment options, we strive to achieve optimal outcomes and improve quality of life.
Surgical Consultants of Central Florida Services
Diagnosis of Fecal Incontinence and Bowel Control Problems

Diagnosing fecal incontinence and bowel control problems typically involves a thorough assessment beginning with a detailed medical history and physical examination to understand symptoms and potential contributing factors. This comprehensive approach allows our providers at Surgical Consultants of Central Florida to accurately diagnose bowel control problems and tailor effective treatment plans for each patient's needs.

Behavioral and Lifestyle Changes for Fecal Incontinence
Conservative management of fecal incontinence includes dietary modifications, pelvic floor exercises, and behavioral therapies designed to improve bowel control and quality of life. Learn about the benefits of fiber-rich diets, specialized training programs, and biofeedback techniques that can help strengthen your pelvic muscles and enhance anal sphincter function. Explore practical strategies to address symptoms and gain confidence in daily activities without the need for invasive procedures.

Medications for Fecal Incontinence
Anti-diarrheal agents like loperamide can be effective in reducing stool frequency and urgency, helping to provide better control over bowel movements. Bulk-forming agents, such as fiber supplements like psyllium, work by firming up stool and regulating bowel consistency, which can alleviate symptoms. For individuals experiencing constipation-related incontinence, gentle laxatives may help maintain regular bowel movements without worsening symptoms. Additionally, topical treatments, including ointments and creams, are useful for protecting the skin and reducing irritation associated with chronic leakage. Learn how these medications function, their potential side effects, and how they can be incorporated into a comprehensive treatment plan to effectively manage fecal incontinence

Advanced Therapies for
Fecal Incontinence
Advanced treatments include innovative procedures and technologies designed to offer improved outcomes when conservative methods fall short. Sacral nerve stimulation involves implanting a device that sends electrical impulses to the sacral nerves, enhancing bowel control and reducing incontinence. Another option, the artificial bowel sphincter, is a surgically implanted device that mimics the function of the anal sphincter to help maintain continence. For some, injectable bulking agents, which are administered to thicken and support the anal canal, can provide additional control. Additionally, more complex surgical interventions, such as sphincteroplasty or bowel reconstruction, may be considered based on individual needs. Learn how these advanced treatments work, their benefits, potential risks, and how they might fit into a personalized management plan for fecal incontinence.
THE INTERSTIM EVALUATION:
A Simple Test Will Let Us Know If This Treatment Is Right For You
15 minute test procedure at our clinic
Evaluate the therapy to see if it is right for you
Strongly Recommended by the American College of Colorectal Surgeons
Nearly 89% of patients with successful outcomes
TESTIMONIALS
What Are Our Patients Saying ?

Surgical Consultants of Central Florida gave me my life back! My world revolved around the bathroom until I found Dr. Oraedu.
Linda Williams
I went from leaking 10 times daily to being completely continent. Thank you to the entire team at Surgical Consultants of Central Florida
Martha Finley
Our Team

Colorectal Surgeon and Bowel Control Specialist
Dr. Christian Oraedu

Office Manager and Medical Assistant
Melissa

Clinic Receptionist and Medical Assistant
Jane Doe
FAQS
What is Fecal Incontinence?
Fecal incontinence is a medical condition characterized by the involuntary loss of stool, leading to an inability to control bowel movements. This can range from occasional leakage to complete loss of control, significantly impacting a person's quality of life and emotional well-being. It may be caused by various factors, including muscle damage, nerve issues, or underlying health conditions. Treatment options vary depending on the severity and underlying causes, and can include lifestyle changes, medications, or surgical interventions to help restore bowel control and improve overall quality of life.
What are the different treatment options for Fecal Incontinence?
Treatment options for fecal incontinence vary based on its severity and underlying causes. They generally fall into three main categories.
Conservative treatments include dietary adjustments, such as increasing fiber intake to solidify stool, and implementing bowel training techniques to establish a regular schedule. Pelvic floor exercises, like Kegels, can strengthen the muscles involved in bowel control. Medications may also be prescribed to manage symptoms, such as anti-diarrheal drugs or stool bulkers. Non-surgical interventions can involve therapies such as biofeedback, which helps retrain the muscles and improve control by providing real-time information on muscle activity. Another option is sacral nerve stimulation, where a device is implanted to send electrical impulses to nerves controlling bowel function, aiding in the improvement of control. In more severe cases, surgical options might be considered. These can include procedures to repair or strengthen the anal sphincter, or more advanced techniques like the implantation of an artificial bowel sphincter or a colostomy, where a portion of the colon is diverted to an external bag. Surgical options are typically explored after conservative and non-surgical treatments have been evaluated.
Each treatment plan is tailored to the individual, aiming to restore bowel control and enhance quality of life.
How does sacral neuromodulation work?
Sacral neuromodulation involves implanting a small device, similar to a pacemaker, under the skin of the buttocks. This device sends electrical impulses to the sacral nerves near the tailbone, which control bowel and pelvic floor muscles. What makes sacral neuromodulation unique is its ability to effectively treat fecal incontinence that do not respond to other therapies. A trial phase precedes permanent implantation, during which the device is temporarily placed to assess its effectiveness in alleviating symptoms. This trial phase allows patients and doctors to determine if sacral neuromodulation is suitable and beneficial before committing to long-term treatment. It offers a reversible option with adjustable settings, providing personalized treatment for improved bowel control and quality of life.